
Medical billing is the process of submitting and following up on claims with health insurance companies in order to receive payment for services rendered by a healthcare provider.
This task involves several individuals, including:
- Office administrators
- Receptionists
- Medical billers
- Medical coders
It is important for any medical practice to know how the medical billing process works in order to avoid facing several problems related to the process.
Six Steps Involved in the Medical Billing Process
Effectively (doing the right thing) and efficiently (doing the thing right) while handling the following steps in the medical billing process is crucial for the success of your revenue cycle.
Step 1: Patient Check-In
The medical billing process starts the moment the patient requests an appointment with the physician. From here, the receptionist or front desk officer gathers patient information, which includes the following:
- Name
- Address
- Birthdate
- Contact number
- Reason for visit
- Insurance provider
- Policy number
It is important to accurately encode this information into the EHR system. Any wrong data encoded may be a cause for a denied or rejected claim in the future.
Step 2: Confirming Insurance Eligibility of the Patient
After recording or updating the initial information, the patient’s insurance coverage should be verified by the office administrator. This includes identifying the list of services covered in the patient’s current insurance policy. The administrator should also be aware of the different billing procedures required by a provider, such as the need for pre-authorization prior to billing.
Once these things have been clarified, the office administrator needs to inform the patient if he or she needs to pay out of pocket for certain services.
Step 3: Handling the Patient Check-Out
All services rendered for the patient must be recorded and placed into the patient’s medical record. This means translating all the diagnoses and medical procedures into medical codes. This is where medical coders enter the picture.
Medical coders determine the diagnoses of the treatments that have been administered to the patient. This is then translated using the ICD or CPT code and encoded into the patient’s ledger.
Here, the patient’s bills, including previous balances (if any) and new charges, are input in relation to any payments the patient or patient’s provider may have paid, all of which are printed and given to the patient in the form of a receipt.
Step 4: Accurately Transmitting the Medical Claim
Now that the diagnoses and treatment services have been properly coded, it is time for the billers to transmit the medical claim to the insurance provider. However, before this is transmitted, it needs to be reviewed internally. This means adhering to written standards and procedures designed by your organization to reduce erroneous claims and fraudulent activity.
This ensures all data has been accurately entered electronically into provider’s system through a clearinghouse or directly to the provider, such as Medicaid.
Step 5: Receiving the Payment
Once the medical claim is received by the insurer, it is reviewed and evaluated. The insurer determines if the entire or just a portion of the bill should be paid, or if it should be denied. All of this depends on the policy and the contract the patient signed with the insurer.
Step 6: Billing the Patient
There are instances wherein the patient needs to pay for the remaining bill not covered by the provider. This is the reason why some insurers and healthcare providers implement a co-payment policy.
If the patient fails to pay the bill accordingly, it is the responsibility of the healthcare provider to followup with the patient through a collection process. Thus, it is important to explain to the patient upfront about the entire medical billing process.
Learn more medical billing tips. Subscribe and follow our blog today.
About ClaimCare
ClaimCare provides a complete solution for all your medical billing concerns. This includes claim submission and follow-up processing, practice analytics and recommendations, instant payment program, automated insurance verification, and patient checkout tool. Learn more about the services we deliver. Complete our online form to schedule an appointment with us.


 Looking back, to look ahead: With ICD-11 on the horizon for 2022,
Looking back, to look ahead: With ICD-11 on the horizon for 2022,  On December 15, 2015, Jason Adam Townsend, owner of a medical billing company, was indicted on
On December 15, 2015, Jason Adam Townsend, owner of a medical billing company, was indicted on  Some of the crucial elements in the medical claims process happen during the medical coding and medical billing procedures.
Some of the crucial elements in the medical claims process happen during the medical coding and medical billing procedures. Is your in-house medical billing costing more than you can handle? How is this compromising your organization's efficiency?
Is your in-house medical billing costing more than you can handle? How is this compromising your organization's efficiency? Last July, the Centers for Medicare and Medicaid Services (CMS) released a proposed payment rule for the Ambulatory Surgery Center Association (ASCA) and Hospital Outpatient Departments (HOPDs) for 2019. These updates address several long-requested ASCA priorities, which include the following:
Last July, the Centers for Medicare and Medicaid Services (CMS) released a proposed payment rule for the Ambulatory Surgery Center Association (ASCA) and Hospital Outpatient Departments (HOPDs) for 2019. These updates address several long-requested ASCA priorities, which include the following: Denial of claim is defined in the
Denial of claim is defined in the 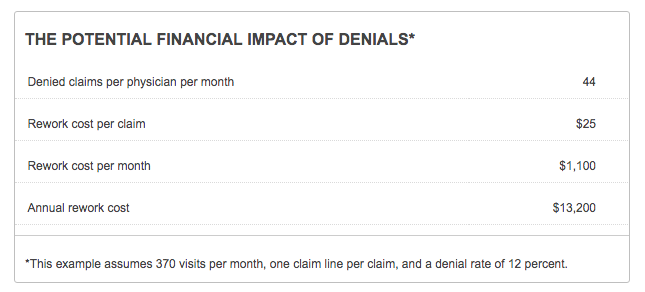
.jpg?width=300&name=Final-puzzle-piece%20(003).jpg) We recently discovered that a new client had just hired an office worker who had a good knowledge of general billing but no experience whatsoever with medical billing. This posed a problem that we solved by meeting with the office worker and explaining some medical billing specifics.
We recently discovered that a new client had just hired an office worker who had a good knowledge of general billing but no experience whatsoever with medical billing. This posed a problem that we solved by meeting with the office worker and explaining some medical billing specifics.