 In dealing with the complexity of the medical credentialing process, some healthcare providers still rely on spreadsheets, checklists, and makeshift programs without an expert to verify these entries. This results in several enrollment errors and delays.
In dealing with the complexity of the medical credentialing process, some healthcare providers still rely on spreadsheets, checklists, and makeshift programs without an expert to verify these entries. This results in several enrollment errors and delays.
Some practices have no dedicated team to handle the credentialing process. Thus, their staff is left juggling their intended responsibilities with other tasks, which only results in inefficiencies and delayed enrollments.
Outsourcing your medical credentialing helps eliminate these problems while offering the following benefits:
- Reduced operating and administrative costs
- Reduced errors in the enrollment and credentialing process
- More time to focus on building your practice
Recent ClaimCare blogs provide in-depth information on why Proper Medical Credentialing is a Vital Necessity and How to Avoid Delays and Mishaps in the credentialing process of verifying your medical staff information regarding:
- Education and certifications
- Training and work experience
- Other professional qualifications
This is vital because unless a physician is enrolled your practice cannot file medical claims for the services he or she delivers. This means no revenue generated for your practice or facility.
Medical Credentialing and the Rising Administrative Costs in the HealthCare Industry
The administrative expense in the US accounts to 8% of healthcare costs. This includes activities related to planning, regulating, and managing health systems and services such as medical credentialing.
Kevin Schulman, a professor of Medicine at Duke and co-author of the "Administrative Costs Associated with Physician Billing and Insurance-Related Activities at an Academic Health Care," shares the reason behind this in the following statement:
"The extraordinary costs we see are not because of administrative slack or because healthcare leaders don’t try to economize. The high administrative costs are functions of the system’s complexity."
One source of this complexity is the multiplicity of payers in the American health system. This includes private insurances and several public health programs such as Medicaid and Medicare.
With the variety of processes required by these payers resulting in increased administrative costs, the healthcare industry needs to consider all the possible cost-reduction solutions for operational efficiency. This includes choosing a third-party provider to handle your medical credentialing process.
Medical Credentialing Outsourcing for Reduced Administrative Costs and Better Patient Care
Below are three ways on how medical credentialing outsourcing can benefit your practice:
1. Reduced Operational and Administrative Costs through Medical Credentialing Outsourcing
In an article published in the Harvard Journal of Medicine, David Cutler Ph.D, Elizabeth Wikler B.A., and Peter Basch, M.D. shared that streamlining your electronic transactions, standardizing your reporting requirements and provider enrollment, and the credentialing system is one of the best solutions to your cost concerns.
How much savings are we talking about? It is estimated to be $29,000 per physician in a year.
2. Reduced Errors Resulting in a Faster Medical Credentialing Process
With a third-party provider, you are working with expert medical staffers who are skilled and knowledgeable regarding all the recent updates on the medical credentialing process. This ensures your enrollment submission has minimal to zero errors.
As a result, you have a faster enrollment process that allows your practice to earn more revenue.
3. More Time to Focus on Building Your Practice
On average, a U.S. physician spends an average of 43 minutes each day on health plan administrative functions. This is equivalent to 261 hours of saved time in a year (365 days).
Now you can say goodbye to these administrative functions because an outsourced medical credentialing provider will do it for you. Your time can be used to focus on building your practice while delivering better services to your patients.
About ClaimCare
ClaimCare is one of the largest medical billing and medical credentialing providers in the United States. Its medical credentialing staff is thoroughly screened, well trained, and provided with the best tools and proper incentives to ensure you are given the best services. For more information about the services we deliver, phone us at (855) 376-7631 or subscribe to our Medical Billing Blog.

 According to a
According to a  An American College of Physicians (ACP) paper titled "Putting Patients First by Reducing Administrative Tasks in Health Care” estimated the annual costs for excessive administrative tasks total $40,069 per full-time equivalent (FTE) physician.
An American College of Physicians (ACP) paper titled "Putting Patients First by Reducing Administrative Tasks in Health Care” estimated the annual costs for excessive administrative tasks total $40,069 per full-time equivalent (FTE) physician. The
The  The majority of the chief financial officers (CFOs) involved in the
The majority of the chief financial officers (CFOs) involved in the 
 In the interest of improving security, Medicare has released new cards meant to prevent identity theft among its users.
In the interest of improving security, Medicare has released new cards meant to prevent identity theft among its users.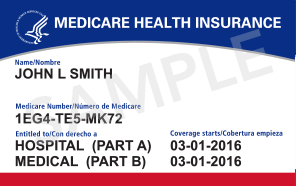
 Medicare has over 200 reason and remark codes they use daily in the process of adjudicating claims. They have recently released the top reasons for
Medicare has over 200 reason and remark codes they use daily in the process of adjudicating claims. They have recently released the top reasons for  If you accept Texas Medicaid then please note the following
If you accept Texas Medicaid then please note the following  Physicians continue to see their collections, cashflow and emotions whipped around like a rag doll in the mouth of a rottweiler. Congress failed to act before the June 1, 2010 deadline. Once again physicians are "officially" under a new Medicare fee schedule that has an average reduction of over 21%. In reaction, Medicare will once more hold claims for the first 10 business days of the month (for June dates of service).
Physicians continue to see their collections, cashflow and emotions whipped around like a rag doll in the mouth of a rottweiler. Congress failed to act before the June 1, 2010 deadline. Once again physicians are "officially" under a new Medicare fee schedule that has an average reduction of over 21%. In reaction, Medicare will once more hold claims for the first 10 business days of the month (for June dates of service).