 In the interest of improving security, Medicare has released new cards meant to prevent identity theft among its users.
In the interest of improving security, Medicare has released new cards meant to prevent identity theft among its users.
The Centers for Medicare & Medicaid Services (CMS) have given physicians and medical billing companies 21 months to fully implement the necessary changes to their medical credentialing and medical billing services. The announcement was made to allow companies the chance to fully comply with the newly implemented Medicare ID card requirements.
The question is, what kind of impact will these new changes have on your billing system and services? What would be the best way to go about this transition? Let’s start by understanding the major changes with the new Medicare ID card...
There are three primary differences in the new Medicare ID card that should be taken note of:
- The removal of the Social Security Number (SSN)
- The replacement of the Health Insurance Claim Number (HICN)
- The use of the Medicare Beneficiary Identifier (MBI)
What’s the major difference between the Medicare Beneficiary Identifier (MBI) and the Health Insurance Claim Number (HICN)?
Previous Medicare cards used to have the SSN based Health Insurance Claim Number (HICN) and used it as a primary identifier for card holders. However, due to rising incidence of identity theft and fraud risks, the Medicare Access and CHIP Reauthorization Act required the CMS to remove the HICN.
Instead, Medicare cardholders will now be provided with a NEW Medicare Beneficiary Identifier (MBI) that features an 11-character-long combination of numbers and uppercase letters (except for S, L, O, I, B and Z), separated by dashes.
It is a unique, non-intelligent and randomly generated sequence of numbers and letters that do not have any special meaning whatsoever.
How will this impact doctors and medical office managers in billing and compliance services?
Currently, the new Medicare cards are already being mailed and distributed to recipients. This means that cardholders will soon be visiting medical offices with their new cards, asking for further clarification about the changes, and seeking assistance for its use. It’s important, therefore, that you are fully prepared to address their concerns, inquiries, and demands.
With this in mind, here are the top three concerns or challenges that you need to take note of given this new policy:
1. Eligibility Verification of the New Medicare ID Card
With the new card, one of the primary concerns that you will have to face will be verifying its authenticity and validity.
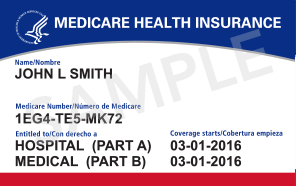
The new card shares the same white, blue and red color like the previous one. However, take note of the new Medicare Number and how it is comprised of uppercase letters and numbers alone. Thus, it is most important for doctors and medical office managers to learn how to identify a valid Medicare ID card from a fraudulent one.
This sounds simple, right? But wait a minute. This is just the tip of the iceberg. There is more information pertaining to the patient’s screening process that has to be verified. This includes:
- Effective dates
- Benefits and calculations
- Administration, follow-up and plan execution
Should there be a need to verify the validity of the card, doctors and medical office managers can check and verify using Medicare Administrative Contractors (MAC's) secure portal, beginning June 2018.
2. Coordination of Benefits with the New Medicare ID card
The major change happening with the new Medicare ID card is the use of the MBI number. CMS is not expecting any other major changes aside from this, unless there are disputes on an individual's account.
Another issue you may encounter is your patients not being able to receive their new Medicare ID cards due to a change of address. How should you handle this if they visit your office and continue to hand over the old Medicare ID card?
To that end, doctors and medical office managers should be proactive and update their records. This is to easily and quickly claim their payments while avoiding unwanted mishandling of client records in the future.
3. Submission of medical claims using the MBI
The issuance of new cards was driven by a need to protect users from potential identity theft and fraud. This basically means that the new Medicare IDs will still require doctors and medical office managers to thoroughly process claims. It’s important, therefore, to ensure that the process and submission of these medical claims are accurate, otherwise you will leave yourself vulnerable to payment delays.
Bottom line…
To help you with this transition, you need to have an efficient system set up that can handle new information, securely handle data, and manage operational efficiencies easily.
ClaimCare provides doctors and medical office managers a complete medical billing solution to manage this transition.
Claim Care:
- provides the top service level guarantee in the industry
- offers best-of-breed technology
- is based 100% in the USA
- an air tight medical billing process
- provides actionable reporting and broad experience
- can work on its clients' medical billing systems.
For more information contact ClaimCare Medical Billing Services by email at sales@claimcare.net , by phone at (855) 376-7631 or visit the ClaimCare Medical Billing Company website.
