 Medical billing reports are important in evaluating the efficiency of your practice. Thus, reports should show the performance of your organization in full details. This will greatly help in improving your revenue cycle.
Medical billing reports are important in evaluating the efficiency of your practice. Thus, reports should show the performance of your organization in full details. This will greatly help in improving your revenue cycle.
Some of the questions reports should be able to answer include:
- Referring physician profitability
- Front desk employee effectiveness
- Payer contractual compliance
- Provider productivity
- Coding profiles
How is this possible? Read on to know the different data analytics that should be present in your medical billing report.
1. Accounts Receivable Aging Report
This report contains any accounts receivable (A/R) that remain to be paid by the insurance companies. It also reveals how long A/R has been unpaid and the average time a claim needs before it is paid by the insurance provider.
As an example, for CIGNA HealthCard holders, Cigna says they do their best to process medical claims within 5 days after filing.
Five days may not be possible, but medical claims should be paid in less than 45 days. Thus, any claim that extends beyond 45 days to be paid should immediately be monitored. If this reaches 90 days, then it is a red sign that you should urgently take action with it.
As a friendly note, you should also consider the type of claim you are requesting. Generally, the following claims take longer to be processed:
- Workers compensation
- Car accident claims
- Out-of-state claims
Thus, it is best to be mindful of any healthcare services provided under this category.
2. The Key Performance Indicators (KPI) Report
Just like any business, your practice should know the most profitable procedures in your organization. Thus, your key performance indicator report should be able to track the following:
- Frequency a procedure is performed
- Sum charges and collection
- Total adjustments
- Outstanding A/R
This should be neatly presented in a document so you can easily compare results on a per-date basis. Any sudden surge or leap in weeks or days should be carefully noted so you can monitor these dates more meticulously.
3. The Insurance Analysis Report
This lists the top payers and insurance companies contributing to your practice, based on the collection per Total Relative Value Unit (RVU).
But what exactly is an RVU?
This represents the following components:
- Physician work expenses: 52%
- Practice expenses (staff, facilities, overhead): 44%
- Malpractice expenses: 4%
It is further influenced by the area of the country in which the service is provided. This, together with the above components, comprises the total RVU of a particular service.
Why is this important for your practice?
Knowing the collection per total RVU of your procedures gives you the leverage to negotiate for better pricing with various insurance companies.
How do you know if you are making a smart negotiation?
Ideally, the collection per Total Relative Value Unit should be higher than the current Medicare Conversion Factor, which is $36.04. If this is lower, then you are not collecting the right amount for your services.
Check who among your payers are paying less and start talking to them about it. If they will not settle with an agreement, then it may be better to drop them and add another carrier that pays better. However, be extra careful before dropping one of your carriers because it may have an impact on your practice.
For better results, seek the advice of experts in the field of medical billing and coding to help you make an assessment of your current medical billing reports.
Do you wish to know more about medical billing and coding practices? Subscribe to our blog for more helpful insights or complete our online form so we can schedule an appointment with you. You may also contact us at (855) 376-7631.
About ClaimCare
ClaimCare delivers medical billing and coding reports with detailed information for you to fully understand the state of your practice. This helps your organization to create action plans that can help improve your performance. It also comes with an easy-to-use dashboard reporting system, which easily presents critical information in a comprehensive manner.

 Looking back, to look ahead: With ICD-11 on the horizon for 2022,
Looking back, to look ahead: With ICD-11 on the horizon for 2022,  The famous Chinese philosopher Confucius once said, "A man who does not plan long ahead will find trouble at his door." This is true, especially with healthcare providers in the U.S. and their physician credentialing process.
The famous Chinese philosopher Confucius once said, "A man who does not plan long ahead will find trouble at his door." This is true, especially with healthcare providers in the U.S. and their physician credentialing process. On December 15, 2015, Jason Adam Townsend, owner of a medical billing company, was indicted on
On December 15, 2015, Jason Adam Townsend, owner of a medical billing company, was indicted on  Some of the crucial elements in the medical claims process happen during the medical coding and medical billing procedures.
Some of the crucial elements in the medical claims process happen during the medical coding and medical billing procedures. Is your in-house medical billing costing more than you can handle? How is this compromising your organization's efficiency?
Is your in-house medical billing costing more than you can handle? How is this compromising your organization's efficiency? Beckers Hospital Review
Beckers Hospital Review Last July, the Centers for Medicare and Medicaid Services (CMS) released a proposed payment rule for the Ambulatory Surgery Center Association (ASCA) and Hospital Outpatient Departments (HOPDs) for 2019. These updates address several long-requested ASCA priorities, which include the following:
Last July, the Centers for Medicare and Medicaid Services (CMS) released a proposed payment rule for the Ambulatory Surgery Center Association (ASCA) and Hospital Outpatient Departments (HOPDs) for 2019. These updates address several long-requested ASCA priorities, which include the following: Denial of claim is defined in the
Denial of claim is defined in the 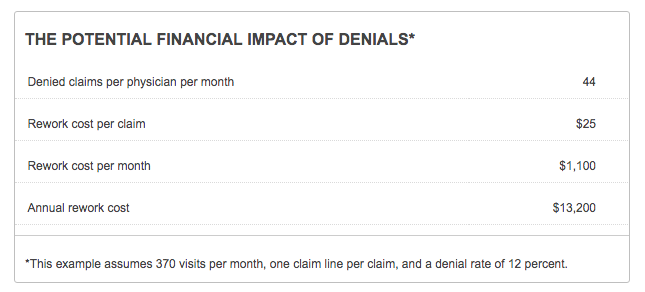
.jpg?width=300&name=Final-puzzle-piece%20(003).jpg) We recently discovered that a new client had just hired an office worker who had a good knowledge of general billing but no experience whatsoever with medical billing. This posed a problem that we solved by meeting with the office worker and explaining some medical billing specifics.
We recently discovered that a new client had just hired an office worker who had a good knowledge of general billing but no experience whatsoever with medical billing. This posed a problem that we solved by meeting with the office worker and explaining some medical billing specifics.