 No enrollment means no payment.
No enrollment means no payment.
When a new physician joins your practice, it is of utmost importance for your practice to expedite his or her medical credentialing and enrollment process. Credentialing specialists at ClaimCare can help you do this effectively (doing the right thing) and cost efficiently (doing the thing right).
Having a fast and reliable medical credentialing process is important.
As you are probably aware, only after a health plan has awarded your new hire with an "effective date of participation" can this physician’s claims be properly submitted for payment.
How much are you losing?
A disrupted cash flow for your practice occurs when an “uncredentialed” physician cannot receive payments for claims while waiting for the practitioner to be enrolled with patients’ health plans.
According to various reports, approximately $30,000 in lost revenue happens to an average primary care physician with just a month of credentialing delays. This amount increases substantially for higher billing specialties such as cardiothoracic surgery and orthopedics.
3 reasons to outsource your medical credentialing and enrollment process:
1. It helps reduce costs while safeguarding stored data.
Allowing a third party medical credentialing provider to handle the enrollment and credentialing process lowers your expenses. It allows you to utilize top-rated hosting and security technology without the need to pay for the installation, implementation, and maintenance of servers and data encryption software.
2. It brings better efficiency through robust Key Performance Indicators.
Third party medical credentialing providers give your practice efficient tracking, trending and reporting data. This includes the following:
- In-process charges
- Department processing times
- Provider process times
- Days in Enrollment (DIE)
- Quality measurements for updating payer follow-up notes
This data allows you to easily establish performance baselines that can help improve your practice. This results in an expedited enrollment and medical credentialing process.
3. It reduces medical credentialing and provider enrollment errors.
Third party providers put the credentialing process into a single team that handles the centralized verification office. They are composed of trained, highly skilled, and knowledgeable individuals who are experts in completing your credentialing and enrollment process. This reduces the errors for your practice.
The bulk credentialing approach of third-party providers also makes it easier for your organization to gain a "delegated status". Once acknowledged, you'll have an even faster enrollment and reimbursement process for your practice.
So why continue to wait for 60 to 120 days before your credentialing process is completed if it can be done faster and more efficiently? Subscribe to our blog or call us at (855) 376-7631 to learn more about the medical credentialing process.
About ClaimCare
Healthcare Tech Outlook named ClaimCare as one of the nation’s “Top 10 Medical Billing Companies” in 2018. This honor follows previous such honors, including being ranked in the “Top 5” by the online magazine, Money & Business. We have a proven track record of increasing client collections by 10 to 20 percent. Talk to us to learn more about our medical credentialing services.

 Are medical claims reimbursements getting more challenging for your practice? You are not alone. There are other practices that have suffered the same in past years, and are still struggling with this problem.
Are medical claims reimbursements getting more challenging for your practice? You are not alone. There are other practices that have suffered the same in past years, and are still struggling with this problem. According to a
According to a  An American College of Physicians (ACP) paper titled "Putting Patients First by Reducing Administrative Tasks in Health Care” estimated the annual costs for excessive administrative tasks total $40,069 per full-time equivalent (FTE) physician.
An American College of Physicians (ACP) paper titled "Putting Patients First by Reducing Administrative Tasks in Health Care” estimated the annual costs for excessive administrative tasks total $40,069 per full-time equivalent (FTE) physician. The
The  Medical credentialing for all practitioners in your group is one of the first steps you should think of when starting your own medical practice. This is essential in dictating the financial stability of your organization.
Medical credentialing for all practitioners in your group is one of the first steps you should think of when starting your own medical practice. This is essential in dictating the financial stability of your organization. The majority of the chief financial officers (CFOs) involved in the
The majority of the chief financial officers (CFOs) involved in the 
 In the interest of improving security, Medicare has released new cards meant to prevent identity theft among its users.
In the interest of improving security, Medicare has released new cards meant to prevent identity theft among its users.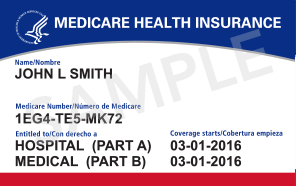
 Until recently physicians believed that they had until January 3, 2011 to comply with Medicare's PECOS enrollment requirement. This is no longer the case. In May Medicare announced that a new mandate from the health system reform law forced the deadline to be moved up by 6 months. Starting July 6, 2010 if the physicians that refer to your practice are not properly enrolled in the Provider Enrollment Chain and Ownership System (PECOS) then your cashflow will be interrupted. If a claim is submitted to Medicare after July 6th with a referring physician that is not enrolled in PECOS, then Medicare can reject the claim. This means that your practice needs to work with your referring provider base and ensure that your referring providers are enrolled in PECOS. This is a much higher burden than the more typical medical billing situation where a provider only needs to ensure the he or she is enrolled with a payer.
Until recently physicians believed that they had until January 3, 2011 to comply with Medicare's PECOS enrollment requirement. This is no longer the case. In May Medicare announced that a new mandate from the health system reform law forced the deadline to be moved up by 6 months. Starting July 6, 2010 if the physicians that refer to your practice are not properly enrolled in the Provider Enrollment Chain and Ownership System (PECOS) then your cashflow will be interrupted. If a claim is submitted to Medicare after July 6th with a referring physician that is not enrolled in PECOS, then Medicare can reject the claim. This means that your practice needs to work with your referring provider base and ensure that your referring providers are enrolled in PECOS. This is a much higher burden than the more typical medical billing situation where a provider only needs to ensure the he or she is enrolled with a payer.