 The majority of the chief financial officers (CFOs) involved in the 2018 CFO Outlook Performance Management Trends and Priorities in Healthcare listed cost reduction as their no. 1 priority.
The majority of the chief financial officers (CFOs) involved in the 2018 CFO Outlook Performance Management Trends and Priorities in Healthcare listed cost reduction as their no. 1 priority.
Among them, 50% expressed the desire for easier report creation, better dashboards and visuals, and enhanced ability to understand the report and data statistics. Also, a staggering 90% have shown their concern over the online payment security of their accounts. How can outsourcing your medical billing services address these concerns? Is this even possible?
How Outsourcing Your Medical Billing Service Can Help Your Practice
Outsourcing your medical billing services can bring numerous benefits to your practice including:
Increased Revenues and Reduced Labor Costs
Approximately, 8% to 10% of medical collections are spent on the medical billing process. However, with an outsourced medical billing, you can:
- Reduce overhead costs
- Increase reimbursements
- Decrease claim denials and rejections
In an orthopedic billing case study, the group reported a 73% increase with their billing revenue within six to eight months. This was due to the improved contracting and exiting unprofitable procedure lines implemented in their medical billing process.
In most instances, physicians and office medical managers even realize a 96% claim payment upon the first submission in less than 45 days. All because they have moved their medical billing services to a third party provider.
Easy to Read Dashboard Reports and Data Statistics
Now you can focus more on your patients rather than spending long hours analyzing and interpreting your medical billing reports, with the help of an outsourced medical billing provider.
Third party providers have medical billing online dashboards that easily show the issues with your medical account at a glance. Also, the data can be tracked on a weekly, monthly, or annual basis according to:
- Patient volumes
- Procedure mixes
- Collections
- Days in AR
This makes it easier for your staff to handle your patients’ financial matters and results in a less time-consuming experience for them.
Safe and Secured Data Infrastructure
Last year, DataBreaches.net shared a data compilation revealing that 477 healthcare breaches affecting 5.579 million patient records were reported to the US Department of Health and Human Services (HHS).
Choosing the services of a well established third party medical billing company can protect your patient records through 100% secure medical billing processes. These HIPAA-compliant providers offer a secure and transparent billing process that ensures your data remains confidential at all times.
Now you can say goodbye to those unwanted cyber hack attacks without having to pay extra for cyber-security protection. These are all taken care of by your third-party provider. All you need is to find a medical billing third-party provider who can deliver the medical billing services you require.
Why Choose ClaimCare for Your Medical Billing Services?
ClaimCare has more than 25 years of experience in medical billing. It has a proven track record of increased customer collection reaching all the way up to 25% (the average increase is approximately 5%) and days in AR under 40 for your collectibles.
Let's talk. Complete our online form or call us toll-free on (855) 376-7631, today.

 In the interest of improving security, Medicare has released new cards meant to prevent identity theft among its users.
In the interest of improving security, Medicare has released new cards meant to prevent identity theft among its users.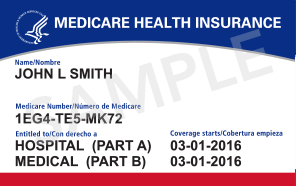
 actices and physician's constantly struggle with understanding how well their billing is working. This can be difficult to do because reliable medical billing benchmarks that can be easily applied are difficult to find. A great solution to this is the use of a
actices and physician's constantly struggle with understanding how well their billing is working. This can be difficult to do because reliable medical billing benchmarks that can be easily applied are difficult to find. A great solution to this is the use of a  Guess what day it is? No, it’s not hump day….it is HIPAA Day! Some providers are taken by surprise! Some practices are under the false impression that they are HIPAA Compliant. Sadly, we are finding more and more that this is not the case.
Guess what day it is? No, it’s not hump day….it is HIPAA Day! Some providers are taken by surprise! Some practices are under the false impression that they are HIPAA Compliant. Sadly, we are finding more and more that this is not the case. Many significant coding and billing changes have been introduced in 2012 for cardiologists, particularly electrophysiologists (EPs). The ClaimCare
Many significant coding and billing changes have been introduced in 2012 for cardiologists, particularly electrophysiologists (EPs). The ClaimCare  ClaimCare, Inc - June 15, 2010 - According to various media reports from Washington, action will come too late regarding the June 6 Senate announcement that it is ready to initiate a 19-month Medicare "doc fix." This means cash-flow problems will affect doctors across the country. Senator Charles Schumer (D-N.Y.) said at a press conference that the Senate is expected to have 60 votes to pass the bill "early next week (week of June 14)." But even if the votes come then, more than likely it will take several days for the bill to be passed by the House and signed into law by the President.
ClaimCare, Inc - June 15, 2010 - According to various media reports from Washington, action will come too late regarding the June 6 Senate announcement that it is ready to initiate a 19-month Medicare "doc fix." This means cash-flow problems will affect doctors across the country. Senator Charles Schumer (D-N.Y.) said at a press conference that the Senate is expected to have 60 votes to pass the bill "early next week (week of June 14)." But even if the votes come then, more than likely it will take several days for the bill to be passed by the House and signed into law by the President.
 Until recently physicians believed that they had until January 3, 2011 to comply with Medicare's PECOS enrollment requirement. This is no longer the case. In May Medicare announced that a new mandate from the health system reform law forced the deadline to be moved up by 6 months. Starting July 6, 2010 if the physicians that refer to your practice are not properly enrolled in the Provider Enrollment Chain and Ownership System (PECOS) then your cashflow will be interrupted. If a claim is submitted to Medicare after July 6th with a referring physician that is not enrolled in PECOS, then Medicare can reject the claim. This means that your practice needs to work with your referring provider base and ensure that your referring providers are enrolled in PECOS. This is a much higher burden than the more typical medical billing situation where a provider only needs to ensure the he or she is enrolled with a payer.
Until recently physicians believed that they had until January 3, 2011 to comply with Medicare's PECOS enrollment requirement. This is no longer the case. In May Medicare announced that a new mandate from the health system reform law forced the deadline to be moved up by 6 months. Starting July 6, 2010 if the physicians that refer to your practice are not properly enrolled in the Provider Enrollment Chain and Ownership System (PECOS) then your cashflow will be interrupted. If a claim is submitted to Medicare after July 6th with a referring physician that is not enrolled in PECOS, then Medicare can reject the claim. This means that your practice needs to work with your referring provider base and ensure that your referring providers are enrolled in PECOS. This is a much higher burden than the more typical medical billing situation where a provider only needs to ensure the he or she is enrolled with a payer.
 Physicians continue to see their collections, cashflow and emotions whipped around like a rag doll in the mouth of a rottweiler. Congress failed to act before the June 1, 2010 deadline. Once again physicians are "officially" under a new Medicare fee schedule that has an average reduction of over 21%. In reaction, Medicare will once more hold claims for the first 10 business days of the month (for June dates of service).
Physicians continue to see their collections, cashflow and emotions whipped around like a rag doll in the mouth of a rottweiler. Congress failed to act before the June 1, 2010 deadline. Once again physicians are "officially" under a new Medicare fee schedule that has an average reduction of over 21%. In reaction, Medicare will once more hold claims for the first 10 business days of the month (for June dates of service).